Autism Breakthrough? Medicare Data to Be Analyzed!
Autism Research Breakthrough? US Health Dept. to Analyze Medicare/Medicaid Data
Introduction: A New Hope for Autism Research?
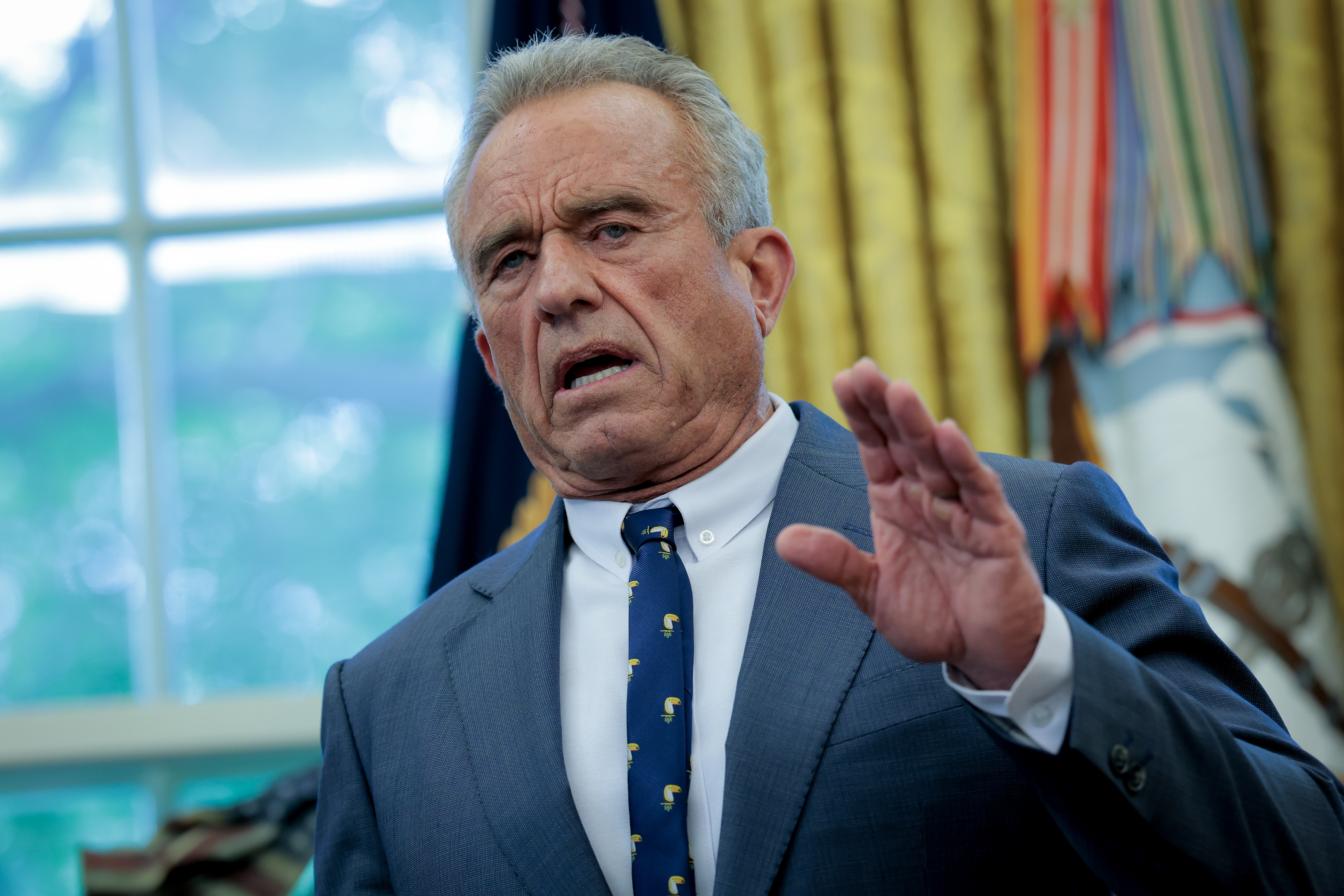
Could we be on the verge of understanding the complexities of autism better? The U.S. Health Department, spearheaded by Secretary Robert F. Kennedy Jr., is embarking on a groundbreaking initiative. They're planning to sift through the medical data of Medicare and Medicaid enrollees to gain insights into autism. Think of it as panning for gold in a vast river of information – hoping to find that one nugget that unlocks a crucial secret.
The Plan: Digging Deep into Data
The core of this ambitious project is a data-sharing agreement. It's a handshake between the National Institutes of Health (NIH), the government's research powerhouse, and the Centers for Medicare and Medicaid Services (CMS). CMS holds the keys to claims data from a staggering 150 million Americans! That's a goldmine of potential information.
Uncovering the Root Causes: Kennedy's Vision
Secretary Kennedy, in a statement, expressed his optimism: "We're using this partnership to uncover the root causes of autism and other chronic diseases." It's a bold statement, filled with hope for a future where we understand and can potentially mitigate the factors contributing to autism.
Privacy First: Protecting Sensitive Information
Of course, with access to such a vast pool of personal data, privacy is paramount. The HHS assures that the agreement will be "consistent with applicable privacy laws to protect Americans' sensitive health information." It’s like having a highly secure vault where the data is stored, only accessible to authorized researchers under strict protocols.
Focusing on Key Areas: Where Will They Look?
The agency plans to focus on several key areas. But what exactly will they be looking for?
Autism Diagnosis Trends: Tracking the Numbers
Analyzing diagnosis trends over time can reveal patterns. Are there geographical hotspots? Are certain demographic groups more affected? Understanding these trends is the first step in understanding the underlying causes. Think of it as mapping the spread of a disease to identify its origin.
Health Outcomes: Understanding the Bigger Picture
It's not just about the diagnosis. How does autism affect overall health? What are the common co-occurring conditions? By analyzing health outcomes, researchers can get a more holistic view of the challenges faced by individuals with autism. It's like looking at the entire ecosystem to understand the role of a single species.
Expert Skepticism: A Dose of Reality
While the initiative is generating buzz, some experts are tempering expectations. They argue that while analyzing data is helpful, it's unlikely to pinpoint the "root causes" of autism. Autism is a complex condition with likely multiple contributing factors, including genetic predisposition and environmental influences. Finding a single "root cause" may be an oversimplification.
The Challenges Ahead: A Long and Winding Road
Identifying the causes of autism is like solving a complex puzzle with thousands of pieces. What are some of the specific challenges researchers face?
Data Interpretation: Making Sense of the Numbers
The sheer volume of data can be overwhelming. Sifting through it to find meaningful patterns requires sophisticated analytical tools and expertise. Are we equipped to handle the amount of data?
Confounding Factors: Untangling the Web
It's difficult to isolate the specific factors that contribute to autism. There are countless variables at play, making it challenging to establish direct cause-and-effect relationships. Imagine trying to separate the individual strands of a tangled web.
Ethical Considerations: Balancing Research and Privacy
Ensuring the privacy and security of sensitive health information is paramount. Stringent ethical guidelines must be in place to prevent misuse of data. How can we ensure data is used responsibly?
Potential Benefits: Why This Matters
Despite the challenges, this initiative holds significant potential. What are some of the potential benefits that could arise from this research?
Improved Diagnosis: Earlier and More Accurate
A better understanding of the underlying causes of autism could lead to more accurate and earlier diagnoses. This, in turn, could enable earlier intervention and support, leading to better outcomes for individuals with autism. Imagine being able to identify autism risk factors in infancy.
Targeted Treatments: Personalized Approaches
Identifying specific subtypes of autism could pave the way for more targeted and personalized treatments. This could lead to more effective interventions tailored to the individual needs of each person with autism. Instead of a one-size-fits-all approach, we could develop individualized treatment plans.
Prevention Strategies: Reducing Risk
If we can identify modifiable risk factors for autism, we could potentially develop prevention strategies to reduce the risk of developing the condition. This could have a profound impact on public health. What if we could modify the exposure to certain environmental factors?
The Role of Funding: Fueling the Research
Adequate funding is essential to support this ambitious research initiative. Will the NIH and CMS have the resources they need to carry out this project effectively?
The Future of Autism Research: A Brighter Tomorrow
This initiative represents a significant step forward in autism research. While the road ahead may be long and challenging, the potential rewards are enormous. With continued dedication and investment, we can hope to make significant progress in understanding and addressing autism. Imagine a future where autism is fully understood, and individuals with autism are empowered to reach their full potential.
Conclusion: A Cautious but Hopeful Outlook
The US Health Department's plan to analyze Medicare and Medicaid data from autistic enrollees is a bold step, albeit one met with cautious optimism from experts. While pinpointing a single "root cause" remains unlikely, this initiative offers a valuable opportunity to identify trends, understand health outcomes, and potentially pave the way for improved diagnosis, targeted treatments, and even prevention strategies. The key will be balancing the pursuit of knowledge with unwavering ethical considerations regarding data privacy. Only time will tell if this data-driven approach will unlock new insights into the complexities of autism, but the effort itself is a testament to the ongoing commitment to understanding and supporting individuals with autism.
Frequently Asked Questions
- Will my personal data be identifiable in this research?
No, the HHS assures that all data will be anonymized and used in accordance with privacy laws. Researchers will only have access to aggregated, de-identified data.
- How long will this research project take?
The timeline for the project is currently unclear, but analyzing such a vast amount of data will likely take several years. Research is an ongoing process, so it will not be a one and done project.
- What specific types of data will be analyzed?
Researchers will be looking at a range of data, including medical diagnoses, treatments received, medications prescribed, and other relevant health information found in Medicare and Medicaid claims data.
- Will this research directly benefit me or my autistic child immediately?
The direct benefits of this research may not be immediate. However, the long-term goal is to improve diagnosis, treatment, and prevention strategies, which will ultimately benefit individuals with autism and their families.
- Who can I contact if I have concerns about my data being used in this research?
<
You can contact the Centers for Medicare and Medicaid Services (CMS) or the National Institutes of Health (NIH) for more information and to address any concerns you may have about the use of your data. You can find contact information on their respective websites.